The scientist from Hong Kong came directly from the airport to the meeting at the National Institutes of Health. There, he told the packed boardroom about a coronavirus outbreak that would become the first pandemic caused by SARS-CoV-1.
Sam Hess, then an NIH postdoc, was in the audience.
“This was before (the news) had hit the mainstream media,” says Hess, a University of Maine professor of physics, remembering the 2002 meeting. “That briefing made a big impression on me, that these things are not something we just read about in textbooks from 1918. These viruses are evolving now. We need to be prepared.”
Hess had been invited to collaborate with renowned NIH biophysicist Joshua Zimmerberg, whose lab was working on HIV, dengue virus, malaria and influenza. And that’s where Hess launched his research in infectious disease, with a focus on the flu.
“I realized we have not defeated infectious disease,” says Hess. “Seeing all this work (in the Zimmerberg lab), it was like, ‘You know what? This is something we need to figure out.’”
Influenza research was well-suited to his physics background, because protein clustering is central to the virus life cycle. Measuring clusters in different ways and understanding how they’re evolving are critical in advancing treatment therapies.
In the last two decades, advances in super-microscopy led by the Hess lab have resulted in new insights — and sights — of influenza particle surface spikes. The surface structures of spike proteins are where the body’s immune response to the virus begins.
Now, in the SARS-CoV-2 pandemic, what Hess and his undergraduate and graduate students have learned about surface spikes on
“Also key is the value of thinking about innovation — knowing that something else is possible, all the time.” Sam Hess
virus particles is contributing to our understanding of the COVID-19 spike protein. The spike protein from the influenza virus is hemagglutinin (HA); the spike protein from the coronavirus is called S. Basically, the spike proteins on the surface of the virus stick or bind to cells in the respiratory tract. Spikes also allow the virus to enter through a process called membrane fusion.
Membrane fusion depends very much on clusters of the spike protein. Hess has been studying that process of how the clusters form, looking at how the host cell might play a role in generating those clusters and, ultimately, how to disrupt that process.
“These clusters are crucial for the infection process, yet nobody knows why they arise,” says Hess. “There were some theories at that time when I first came to UMaine about why clusters of viral proteins occur. Our data showed those theories to be wrong, which didn’t make me very popular. It did lead us to ask new kinds of questions.
“When the coronavirus pandemic started, I realized we’d probably have to find some new ways to fight the new virus,” he says. “There were some similarities and differences that I noticed between the SARS coronavirus and the influenza virus. I thought of using our molecular microscopes to look at similarities and differences between those two. We’ve been looking at two of the most important proteins involved in the beginning of infection — the spike proteins.”
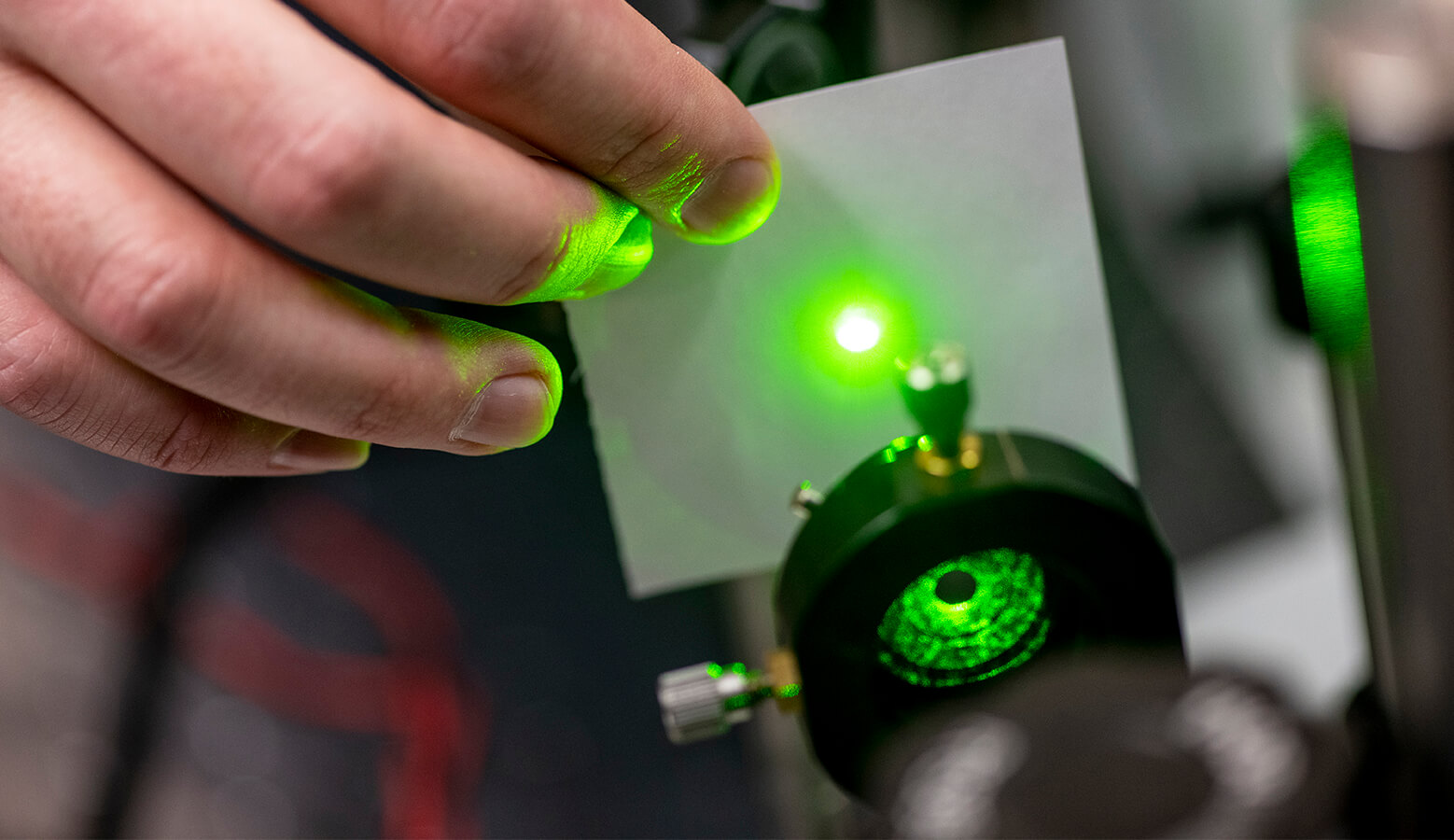
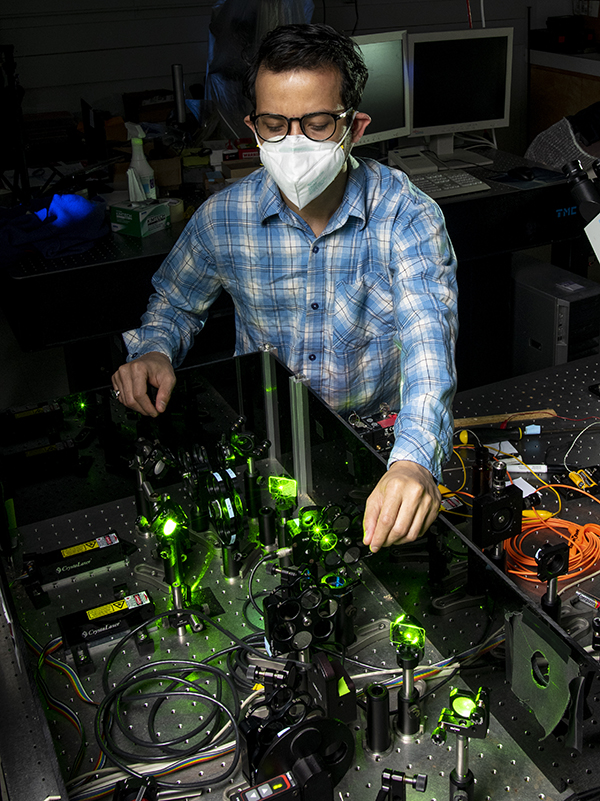
Physics connects to so many things in the world — how things move around and have momentum, and interact with each other. And, importantly, how things interact with light, says Hess, who uses light microscopes to study viruses.
“Physics has allowed us to invent some new kinds of microscopes that can do amazing things,” he says.
In 2005, Hess and UMaine Professor of Chemical and Biomedical Engineering Michael Mason led the development of a breakthrough microscope system called FPALM (fluorescence photoactivation localization microscopy) to image cells with membranes that contain the HA spike protein. Prior to such super-microscopy, it wasn’t possible to create images of molecules on a small enough scale in a living cell to test the biological models that predict how they may be organized. FPALM shattered the resolution limit of lens-based microscopes, known as the diffraction barrier, that had existed for more than a century.
The FPALM system, which uses photoactivatable dyes to identify individual molecules and separate them at the nanometer scale, was one of four groundbreaking advanced microscopy techniques that were able to achieve such single-molecule imaging capabilities in the mid‑2000s. Indeed, announcements of the 2014 Nobel Prize in Chemistry honored three recipients and cited other researchers involved in similar pioneering research, including Hess.
“What we acquire with the microscope is a movie of those flashes of light that occur from different parts of the sample,” Hess says. “Then we use a computer algorithm to look at those images and find where each flash came from. That’s called localization. When we find all those locations of the molecules, then we combine them all together and make a final image out of it.
“We’re taking many, many frames, 10,000 frames, 20,000 frames, from a movie of a single cell or a single area of something. Then we’re making a composite out of all of the locations of the molecules.”
FPALM technology is now used in UMaine research in toxicology and muscular dystrophy. In virology, it has led to not only a better view of spike proteins, but also their cytoplasmic tail, which seems to interact with host cell components connected to signaling.
Parts of those spike proteins mutate fairly rapidly over time, interfering with the function of the immune system to recognize that structure as dangerous and attack it, says Hess. That’s one reason influenza vaccines have to be reformulated annually.
However, there’s a portion of the spike proteins — the tail inside rather than on the surface of the virus — that does not change very quickly. “That,” Hess says, “is what we’re going after.”
“People overlook this tail,” Hess says. “It’s inside the cell. It doesn’t seem to have any role in the lock and key mechanism of entry, but certain sequence elements are always there. In 17,000 different sequences of flu virus, they all had a particular pattern in the tail. If something is unimportant, it’s not going to last like that through every single sequence. I think there is something very important about that. The same features are there in the SARS coronavirus spike.
“We noticed when we expressed one of these spike proteins in a cell that there were some interactions between the tail and some of the host cell components,” Hess says. “Then we started thinking about how we could disrupt that interaction — interfere with the function of the spike protein. Looking at that interaction and trying to figure out if there are drugs that could break that up, that’s been a thrust of our research for a few years.”
The result could be a new class of drugs that blocks this interaction between the spike protein and the host cell, disrupts those clusters of the spike proteins, and stops the virus from entering the host.
“The way viruses are mutating and the way sometimes you get breakthrough infections, having a backup (drug therapy) to help when an infection does occur is a real urgent need right now,” says Hess. “These viruses are quite sneaky. They have redundant mechanisms. You figure out a way to break something and stop it in one way, it adapts to sneak around and infect in a different way. They’re constantly changing.”
“The urgency is there. The coronavirus right now is causing so much trouble. There are great vaccines available to protect us, but the viruses also mutate with time. We’re hoping we can have some kind of a backup. We want to have something to protect us even if infections happen.”
Multidisciplinary research is crucial for tackling these very complex mechanisms of infection, says Hess. The research has involved collaborations with UMaine scientists in physics, chemistry, biology, computer science, engineering and virology, and NIH experts in computer science, biophysics and virology.
“It’s crucial because we don’t all think in the same ways. I might, as a physicist, think about attacking a problem in a certain way. On the other hand, a virologist would say, ‘We need to try this and control for this possibility.’ We’ve also started doing modeling of molecules using computers. That’s something that’s happened since the start of the pandemic for us.”
“The urgency is there. The coronavirus right now is causing so much trouble. There are great vaccines available to protect us, but the viruses also mutate with time. We’re hoping we can have some kind of a backup. We want to have something to protect us even if infections happen.” Sam Hess
Also key is the value of thinking about innovation — knowing that something else is possible, all the time.
“I feel so lucky to have been able to see examples of people who invented things,” says Hess. “My doctoral advisor, Watt Webb, at Cornell was a big influence in that kind of thinking. He invented more than 10 different microscope methods and spectroscopy methods. There was this culture in his group of inventing new ways of doing things. I got to see other people in the middle of that creative process hashing out, ‘Could we do it this way? What about this way?’
“That then led to something that worked out, was a new thing, and was published. That was eye-opening to me. (It’s about) breaking that glass case around the idea of inventing something being inaccessible or too hard. Seeing people do it gave me inspiration,” says Hess, who now models that thinking for the undergraduates and graduate students who have been in his lab.
Students from his lab have gone on to postdoc positions at the Weill Cornell Medical School, Yale School of Medicine, NIH, and into jobs in the biomedical technology sector. That includes a former postdoc from the Hess lab working as a scientist for a company developing super-resolution microscopes using UMaine’s patented technology.
Ongoing improvements in advanced microscopy will one day allow researchers to look at the inner workings of molecules, not just where they are located, Hess predicts. Computer simulations of molecular structure could then be tested with super-resolution technology.
“Those are growing together like trees that were planted separately, but their branches are getting more intertwined,” Hess says. “I think that’s going to continue in the future. I’ve had this philosophy of going after a biological question and trying to invent the technology that I need to answer that question.
“Sometimes, that works out when we get an answer. That answer leads to new biological questions which then lead to new needs. I’ve been trying to keep the technology and the biology walking together and helping each other.
“In the long run, I am quite hopeful that we’re going to be able to find some drugs, find some treatments and maybe even find some cures for these infectious diseases that are causing us trouble right now,” Hess says.
